Health & Medicine
‘The doctors of the lab’
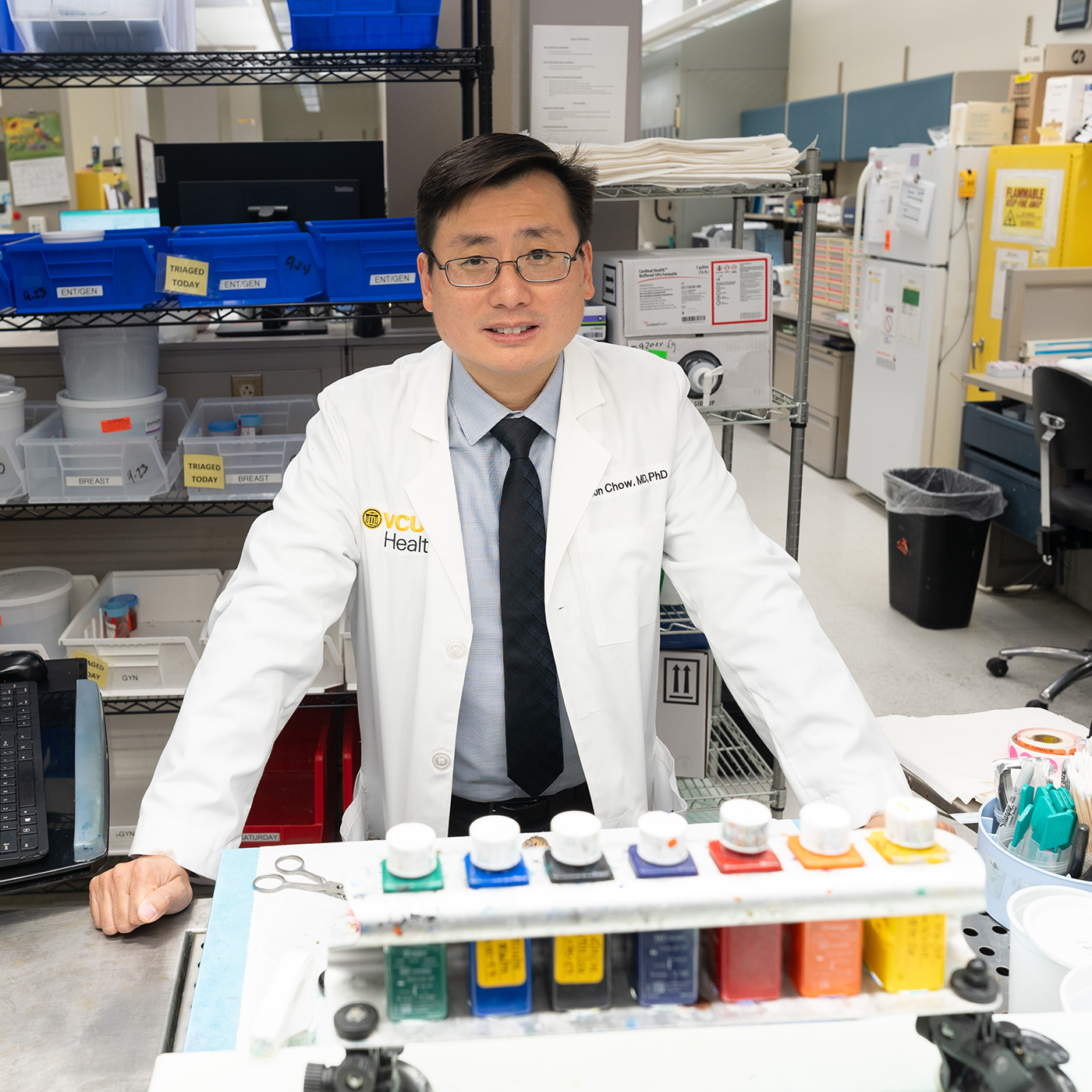
Pathologist Woon Chow brings us into medicine’s diagnostic nerve center.
Woon Chow, M.D., Ph.D., is playing tour guide on the sixth floor of the Gateway Building at VCU Medical Center.
“Ask as many questions as you like,” he says as he walks down the hallway, swipes an ID badge and enters a large laboratory.
Chow (B.S.’03, B.S.’03, M.D.’11, Ph.D.’11, H.S.’15, M.S.H.A.’24) is a neuropathologist and assistant professor of pathology and ophthalmology in the VCU School of Medicine. Today he’s giving the magazine a backstage look at a few of VCU Medical Center’s pathology labs, which run millions of diagnostic tests every year, and are — like so much of health care — evolving rapidly amid a technological golden age for medical science.
“This is our accession area. A tissue specimen comes in, and this is where it starts its journey in the lab,” Chow says, approaching a workstation. “Here, we get pretty much anything — large resections, endometrial biopsies, colon biopsies,
polyps.”
Pathology is one of those fields that almost everyone has encountered but most of us barely fathom: It’s the branch of medicine that uses laboratory methods to diagnose and manage disease. Broadly, there are two subfields: anatomic pathology (tissues) and clinical pathology (fluids). If you’ve had a tumor cut out by a surgeon, a skin tag removed by a dermatologist or been sent for bloodwork after a physical, you’ve been on pathology’s front porch.
It’s in these rooms, though, where the science happens. This is medicine’s diagnostic nerve center, where, in thousands of labs across America, pathologist assistants, medical technicians and the pathologists in charge inspect blood cells, track sodium levels in urine, and cut and stain tissue samples from just about any part of the human body to determine what, if anything, is wrong.
At the anatomic pathology lab’s accessioning stations, the tissue sample gets a case number. From there, it heads to a fridge, where it’s sorted based on organ system; then to a lab bench, where a pathologist assistant, in a step called “grossing,” documents what the specimen looks like and selects smaller samples to later examine under microscope.
Those samples are encased in a block of wax, then sliced with a blade that would make your local delicatessen jealous. Now about four-thousandths of a millimeter thick, the samples are placed on microscope slides and transferred to a container with a clear door. A robot stains each sample purple and pink to make different tissue structures discernable (the tissue itself is colorless) and affixes a coverslip.
Pathologists are “the doctors of the lab,” Chow says. What they observe on the slide leads to a diagnosis. On any given day, VCU’s anatomic pathology lab can generate up to 2,000 slides.
“And you can see how labor-intensive it is,” Chow says. “We have an army of technicians, but you can see the grossing, the tissue processing, getting the section you want, the quality control. All of this takes a day or two, depending on the specimen. And that’s pretty fast.”
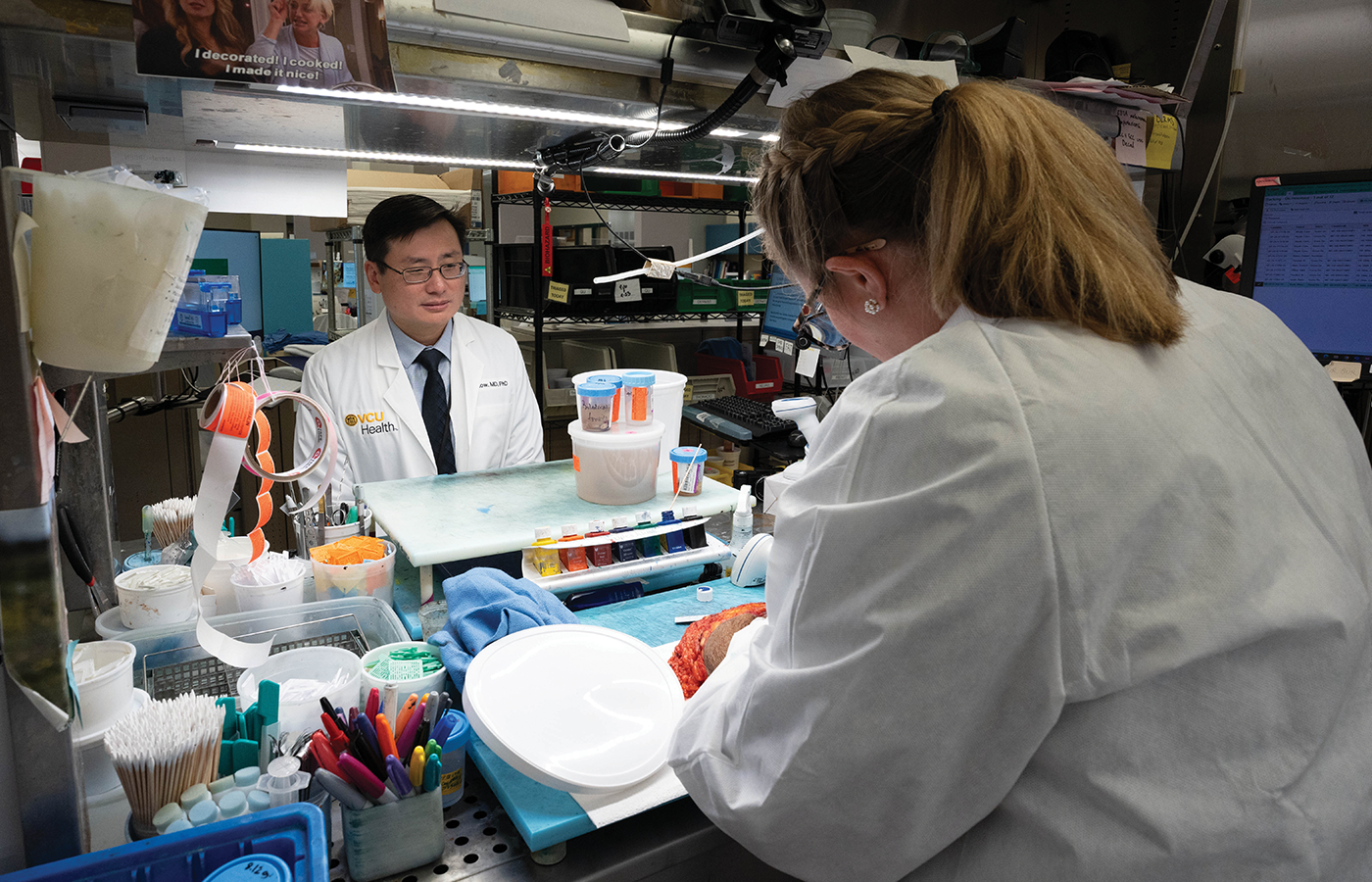
Woon Chow, M.D., Ph.D., and pathologist assistant Emily Nangano in the anatomic pathology lab's accession station. — Jud Froelich (M.S.’21)
Questions about the nature of disease date to Hippocrates (“pathology” roughly translates from ancient Greek as “the study of suffering”). Anatomic pathology’s modern era mostly evolved alongside the microscope, the use of which grew exponentially in the 19th century thanks to improvements in lens making. The process Chow just described — except for assists from the robots and the deli super-slicers — hasn’t changed much since the late 1800s.
At least not yet.
Chow is sitting in his office now — a windowless alcove in the basement of Sanger Hall, across the street from the Gateway Building — and loading a presentation on a set of computer monitors. Behind him is a high table with a large microscope. It’s not the kind you’d find in a high school science class.
He has just examined on that microscope a slide containing an eyeball specimen for a patient with ocular cancer. Chow taps his mouse and pulls up a video.
It’s worth noting here that Woon Chow is a bit of a Renaissance man. He has bachelor’s degrees in physics and biomedical engineering and an M.D.-Ph.D. in neurobiology (all from VCU). He’s the deputy chief health informatics officer for the Central Virginia VA Health Care System. A year ago, he and his wife, Sadia Sayeed, M.D. (H.S.’16), a faculty member in the Department of Pathology, created a scholarship for VCU biomedical engineering students. (It’s named for Chow’s mentor, Joseph Feher, Ph.D., a longtime physiology professor who taught engineering students.) In 2024, Chow earned a master’s in health administration. He’s been studying or working in medical science for 25 of his 43 years on Earth.
Chow begins playing the video. In it, a small glob of tissue rests on a clear stage while a petite scanning laser traces a path on the other side of the glass.
“This is akin to a tissue scanner,” Chow says. It looks like a tiny Roomba. “And this is a piece of tissue, just like upstairs [in the AP lab]. And the detector is scanning it. This is analogous to what we have in radiology now. But here’s the cool thing: Instead of a two-dimensional image, you get a three-dimensional one.”
Chow clicks his mouse. On the screen now is a thick worm of purple-and-pink tissue.
“This is a prostate core. And this is prostate cancer,” Chow says, pointing to the purple areas.
“For the last hundred years or more, all we’ve been doing is looking at cancers or other diseases in two-dimension because that’s all we had,” Chow says. “But in reality all diseases are three-dimensional. We never had the capability to look at this like this before. But now we can.”
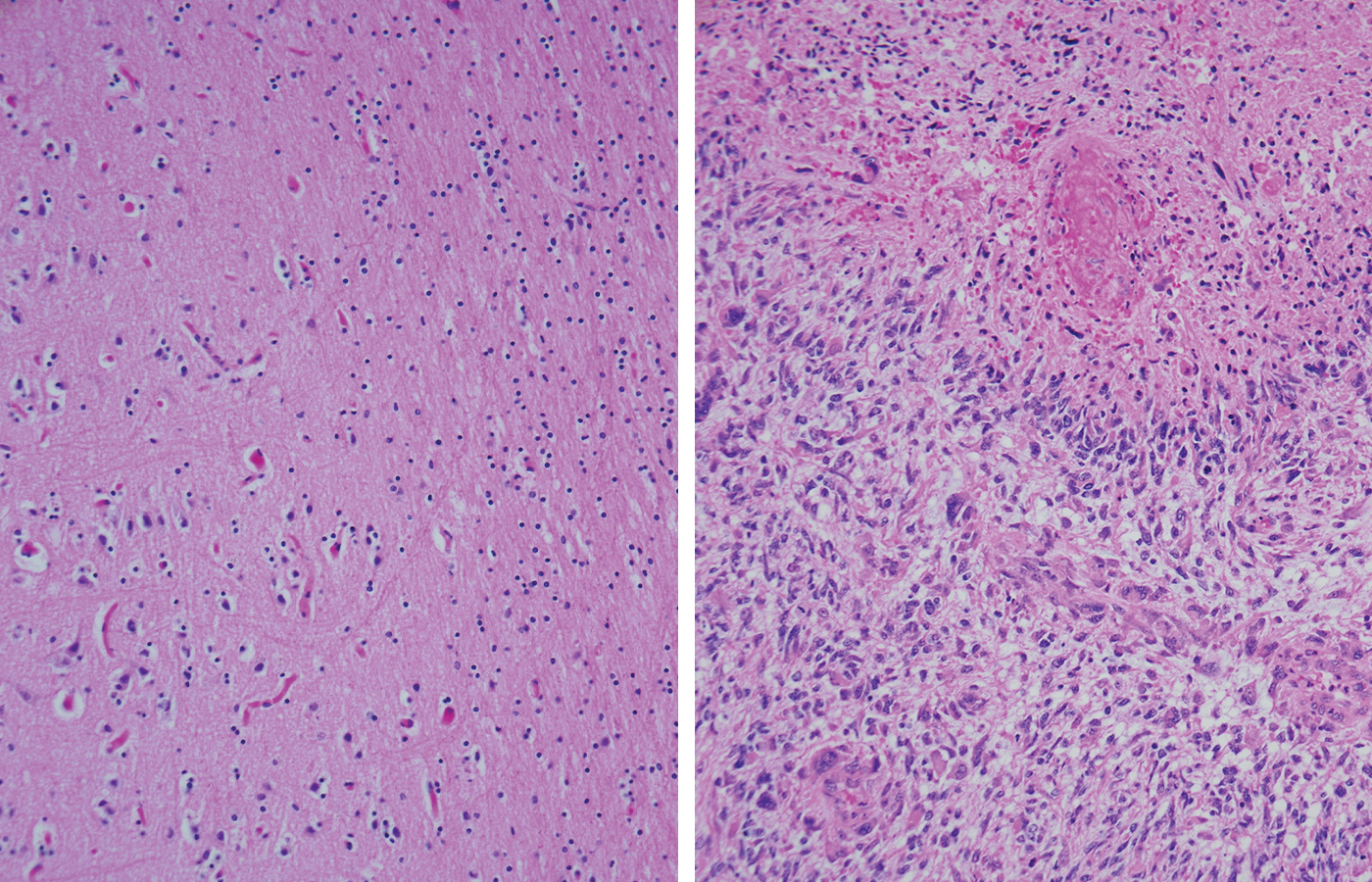
These images show two brain tissue samples. The left shows normal brain tissue; the right shows brain tissue with glioblastoma, a fast-growing cancer.
This is light-sheet microscopy, Chow says. It works by visually dividing tissue samples into thin planes — a sort of digital version of the blade in the AP lab — then stacking those scans to reconstruct the tissue on screen. Though not yet in widespread use as a diagnostic tool, Chow thinks this kind of technology has a lot of potential. He sees a future where tiny scanners can rest on someone’s skin and reveal microscopic mysteries beneath the surface.
“It’s probably the next level, but I don’t think it’s that far-fetched,” he says. “Right now, with radiology, you’re scanning the body and you’re getting an X-ray or an MRI.” Plus, he notes, tissue scanning is nondestructive. “Traditional histology uses up the tissue, and diagnostic testing at times can be limited by small samples. But with scanning, we can generate microscopic images and still use the tissue for other diagnostic tests or even research.”
If Chow seems overly bullish, consider two things: America, with all those labs, has the world’s best diagnostic testing infrastructure. And technology has already revolutionized clinical pathology, AP’s fluid-focused sibling.
Once the domain of medical technicians using pipettes to measure, transfer and analyze samples by hand, CP labs today are bona fide medical Tomorrowlands. In VCU’s lab, algorithms route barcode-labeled test tubes, orchestrating millions of tests a year. Powerful instruments can tally someone’s blood count within minutes. Image analysis software — powered in part by artificial intelligence — can isolate, identify and display individual white blood cells in diseased samples.
“It actually can recognize all the different blood cells. And it’ll put them on a screen,” Chow says. “It can pick out the cells and give you an image so you can see what a blood smear looks like without having to look for all these cells using a microscope. When you have a cancer case, like leukemia, you can see it instantly. And since it’s digitized, it’s easily shareable.
“It’s still not perfect. We still have microscopes; we still have human intervention — which we’ll always need. But the improvements are significant. Just imagine the incredible possibilities and the profound impact these tools will have on patient care as they continue to evolve and combine with other technologies. You can see where this could all go.”
Read more about Woon Chow and the Joseph and Leona Feher Endowed Scholarship for Distinction in Biomedical Engineering at go.vcu.edu/feher-scholarship.
