Research & Discovery
The Magical Mystery Receptor
It’s a new era for psychedelic research. Long-banned drugs like LSD and psilocybin are being reevaluated for their therapeutic potential against depression and addiction. Biochemist Javier González-Maeso is separating the mystical from medical science.
In his fifth-floor office, Javier González-Maeso has a chalkboard, and on this sunny fall afternoon he’s standing at it, diagramming brain magic. At least it would seem to those of us who aren’t affable Spanish biochemists.
González-Maeso, Ph.D., is a 50-year-old professor in VCU’s School of Medicine who’s been funded for 14 straight years by the National Institutes of Health to study the molecular causes of, and treatments for, mental illness and addiction. Originally from the rainy fishing town of Santurtzi in northern Spain, he is, at this November moment, explaining through the elegance of illustration how selective serotonin reuptake inhibitors (SSRIs to the abbreviationally minded) work.
These are the most-prescribed antidepressants on Earth, and as the name tells us, they work by futzing with serotonin levels in the brains of the millions and millions of people worldwide who take them. SSRIs — five are approved for U.S. use, among them Prozac and Lexapro — keep serotonin in the brain by stopping its reabsorption (that’s what “reuptake” means) by neurons, the cellular pathways that would otherwise blast the chemical throughout your central nervous system.
Serotonin is a neurotransmitter, carrying information bodywide along those neurons, and it affects everything from mood to hunger, from sleep to sex drive. Low serotonin levels cause, or at least influence, depression. And while we know what SSRIs do, we don’t really know how. Many scientists consider this annoying.
The drugs’ effects are observable, and the mechanics are mappable. González-Maeso’s chalky art shows how receptors — proteins shaped like alien upside-down pronged antennas — modulate serotonin levels and distribution. But the actual science remains mysterious.
“If someone has, let’s say, cancer, you can get a blood test,” González-Maeso says. “And based on the analysis, they can tell you, ‘You can take this medicine for this disorder and you may respond and you may not respond,’ because you have something that you can use to make the diagnosis. In psychiatry, in general, we don’t have that. The clinicians have interviews. No more. They have interviews with the patients, and based on how the patients behave, they decide if [the patients are] going to receive these antidepressants. And if they don’t respond [to a specific antidepressant], they try another one. But they don’t have any measure they can take from the blood or from anywhere that tells the clinician what medication is going to be the best for the patient.”
Mental illness has been diagnosed and understood largely through these interviews, forcing psychiatrists to act as much like Jedis as doctors when prescribing medication — hence the weeks-later debriefing after starting an antidepressant.
Not only does it take that long for the drugs to do their pharmacokinetic stuff, it’s hard to predict how an antidepressant or its dosage is going to make someone feel. It could make everything a little brighter, not work at all or make you want to lie down in a lonely shadow and cry.
After 70 years or so of biological psychiatry, this is the best we’ve got.
So far.
Biological psychiatry is the name for an increasingly trendy enclave of medical science, dedicated to demystifying the biochemistry of mental illness and addiction, and it’s being pushed by resurgently trendy drugs, their medicinal reputations restored after a 498-page defaming by the Controlled Substances Act of 1971.
This is the psychedelic-therapy renaissance.
“Three or four years ago, it was in the whole U.S., maybe three labs working with psychedelics,” González-Maeso says. “Now psychedelics are almost everywhere.”
Researchers focus largely on the four “classical” psychedelics: psilocybin, LSD (also known as acid) mescaline (you might know it as peyote or from a William S. Burroughs novel) and DMT, the quartet’s most powerful member.
After more than 30 years of here-and-there interest, psychedelics are back from their federal timeout in psychiatric esoterica. Sparked in part by a 2006 Johns Hopkins University study that found that low doses of psilocybin — the psychoactive compound in “magic mushrooms” — improved people’s long-term attitudinal and spiritual well-being, this new era of psychedelic research has grown from niche to status quo.
Psychedelics are nonaddictive — “You have the trip and then you’re done,” González-Maeso says — and generally side effect-free, although psilocybin, depending on how it’s consumed, can cause a little nausea, which manifests as a kind of mild transdimensional flu. SSRIs also can cause nausea, in addition to insomnia, dry mouth, weight gain, fatigue, diminished libido, appetite loss and — no kidding — anxiety.
The big intrigue around psychedelics-as-therapy is their potential to power forth where traditional antidepressants stall out.
Researchers focus largely on the four “classical” psychedelics: psilocybin, LSD (also known as acid) mescaline (you might know it as peyote or from a William S. Burroughs novel) and DMT, the quartet’s most powerful member. It occurs naturally in our brains as well as in certain plants, and the trips are short (15 to 20 minutes), intense and reality-rending.
There’s also interest in classical psychedelic-adjacent drugs, such as MDMA (more commonly known as ecstasy) and ketamine, a synthetic compound used in anesthesia that’s been OK’d by the Food and Drug Administration as a prescription analgesic to treat depression. Ketamine, however, can be addictive.
“People didn’t care much about why these drugs [worked],” González-Maeso says about the 1950s and ’60s, when relevant experts first explored the therapeutic applications of psychedelics, especially psilocybin and LSD (the latter used to treat alcoholism). Back then, research interest centered more on the drugs’ effects than their chemistry. Antidepressants and antipsychotics were developed around the same time.
“But now, with the clinical data that’s very impressive,” González-Maeso says, “many labs are interested in how these drugs induce these clinical effects.
“We have some theories and hypotheses, but almost all the work done is to understand how these drugs induce clinically relevant effects in so many psychiatric conditions.” These include depression, anxiety, PTSD, personality and mood disorders, drug addiction and helping terminally ill patients confront and accept their mortality. And unlike other psychiatric drugs, psychedelics can be effective with a single dose.
González-Maeso’s 10-person lab in the Department of Physiology and Biophysics has its own nook within the greater renaissance, bankrolled with $8.5 million in NIH funding since 2009 — including $1.6 million on the fourth and latest renewal of what was originally a five-year grant — to figure out if the hallucinations these drugs often induce are essential to their therapeutic benefits. He’s concentrated on LSD and now psilocybin, which nowadays are being extensively tested and drawing bedroom eyes from pharmaceutical companies.
About 50 publicly traded companies specialize in psychedelic research, says Kripa Krishman, a senior consultant at Citeline, which analyzes the pharmaceutical industry. The industry’s expected to be worth $8.3 billion by 2028,Krishman says, and the companies’ top priority is drug discovery and development, which is where González-Maeso comes in.
He is studying a particular receptor in the brain, identified 40 years ago as the one that allows us to experience these drugs in all these wondrous ways.
This animal-loving man — he has a dog, a fish tank and a three-legged box turtle — wants to map this receptor’s seemingly numinous dance with psychedelic compounds so someday one of those drug companies can synthesize an antidepressant-style pill that is all therapy and no trip. This should not only reduce the time and cost of psychedelic therapy as it’s currently practiced — weeks of talk therapy to prepare, then a workday-long psychedelic trip proctored by multiple psychologists, costing many thousands of out-of-pocket dollars — it would make this treatment available to people who might not be so hipped to see colors breathe and feel existence tremble.
“I think that the patients who are willing to receive psychedelics do not belong to the general population,” González-Maeso says. “For example, if you tell my grandma, ‘You are sad, go to the hospital and take a piece of one of these drugs’ — you know, she’s not doing that.”
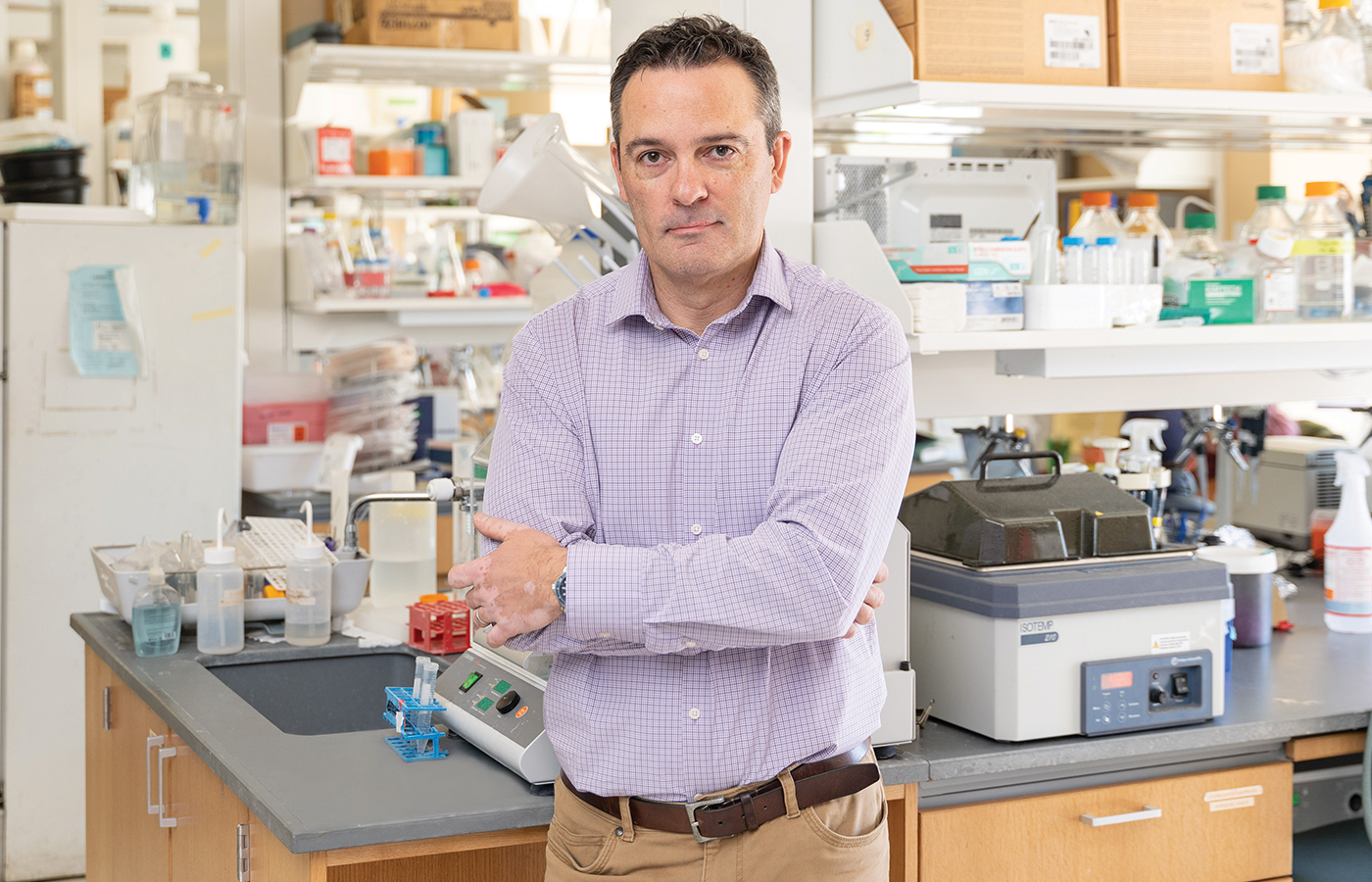
Javier González-Maeso in his lab in the Molecular Medicine Research Building on East Broad Street. He has spent more than 20 years studying how psychedelics interact with our brains. (Jud Froelich)
González-Maeso, like just about everyone else studying this stuff, is enchanted by the serotonin 5-HT2A receptor, proposed by Richard Glennon, Ph.D., in 1984 as the receptor responsible for facilitating psychedelia in our minds and, possibly, our souls.
“If you look at the old literature in the 1950s and ’60s,” says Glennon, a professor emeritus in VCU’s School of Pharmacy (working with Glennon is part of what lured González-Maeso to VCU), “people were suggesting that some of these psychoactive drugs could interact with these certain receptors in the brain, called serotonin receptors. So some people said that they activated those receptors. Others argued they might inactivate the receptors — in other words, act as antagonists. So we got involved in that and — actually there is a book. Oh God, who wrote it? Don’t tell me.”
Glennon is chatting by telephone one late morning from his home office in suburban Richmond. It sounds like a curious place, perhaps with one of those rolling ladders from a Victorian library, a secret slideaway bookshelf and a bow-tied man named Thurmont or Gregory to fetch slippers, newspapers and tea. Glennon pauses to rummage. It doesn’t take long.
“As a matter of fact,” he says, “I have a copy of it right here. ‘Chemical Psychoses’ by Leo Hollister. What he tried to do for the first time was to classify various psychoactive agents … and that included all kinds of things. It included LSD, psilocybin, but it also included, like, THC for marijuana, and a number of other drugs. In other words, anything that affected the brain. And these were all sort of lumped together in one category and what I noticed was that some of them seemed to have an effect on serotonin.”
Glennon is referring to those classical psychedelics, also known as hallucinogens. There are actually a lot of names for these drugs, and the names usually reflect the namers’ point of view. One of these names, “entheogen,” is popular with the mystically enthused. It means “the divine within.” Glennon prefers a barely used term, “psychoheuristic,” devised by the late chemist-psychiatrist Stephen Szára.
“‘Heuristic’ is derived from the Greek word heuriskein, which means to invent or discover,” Glennon says. “Now put it together. ‘Psychoheuristic’ — to discover the mind, the brain. I absolutely love the term” — you can almost hear the man smiling in his library — “but this is the only place it’s ever been mentioned, except in a few articles where I bring it up saying I like this term.”
A more scientific name for these compounds is serotonergic hallucinogen, which just means hallucinogens/psychedelics/[your favorite name here] that interact with the brain through serotonin receptors. Ketamine, for example, doesn’t work through a serotonin receptor but has psychedelic-like effects.
“We started pursuing this serotonin area,” Glennon says, “and what we found was that, yeah, they seem to turn on this serotonin receptor. And then in 1978, it was determined there were two kinds of serotonin [5-HT] receptors in the brain: serotonin1 and serotonin2. So then we started looking at that. We ruled out serotonin1; we ruled in serotonin2 [as being able to interact with psychedelics]. Then over the next bunch of years, it turned out that there are actually seven families of serotonin receptors in the brain, serotonin1 through serotonin7, and some of these had subfamilies. So, like serotonin1, you had 1A, 1B, blah blah blah. It turns out there’s like 15 different kinds of serotonin receptors in the brain, and eventually after looking at a variety of receptors, we pinned it down to the serotonin2A receptor exactly, and this is what we call the 5-HT2A hypothesis of hallucinogenic drug action.”
Each receptor is a prong on those upside-down antennae, which are 3 nanometers long (10 million nanometers equals 1 centimeter) and classified as G protein-coupled receptors. These are molecules on a cell’s surface that bind to a specific substance, including neurotransmitters, hormones and environmental stimulants. These receptor molecules are the targets for nearly half of the drugs currently used to treat human diseases.
If someone (say, our friend Javier working over there on East Broad by the interstate) is able to crack the thus-far recondite biochemistry of these receptors and their psychedelic rapports, it might lead to that all-therapy, no-trip pill that keeps Grandma from dropping acid.
“There’s no question HT2A is involved. There is absolutely no question,” Glennon says. “It’s just what’s going on with the second messengers. In other words, trafficking. That is what is getting people interested. And why is trafficking important? Well, it could be that one of those arms [the prongs on the antenna] produces the hallucinogenic effect, but activation of one of the other arms does not. So the idea is: Can you activate the nonhallucinogenic arm and still produce an antidepressant-like effect?”
This is what González-Maeso wants to do.
“I can understand why your grandmother wouldn’t want to take LSD,” Glennon says. “But if you can make a compound — and that’s why I love medicinal chemistry; it’s chemistry and pharmacology — if you can make a compound that only targets one of those arms, the nonhallucinogenic arm, you could now have something really exciting.”
Here’s why. According to the NIH, in 2021, 57.8 million adult Americans had a mental illness. That’s about 23% of the population. A Centers for Disease Control and Prevention study conducted from 2015 to 2018 found that 13.2% of Americans 18 and older (about 40 million people) had taken an antidepressant in the past month. And in 2020, according to the NIH, about 21 million adults suffered a “major depressive episode.” That constitutes about 8% of the population.
“And about one-third of those have what is called ‘treatment-resistant depression,’” Glennon says. “So your current antidepressants don’t work on them.
“The other thing is, with antidepressants, it takes like four, six, eight weeks for these things to work, and you take them for a long period of time, and people have found with some of these psychedelic agents, you give one or two doses, they work almost immediately. You don’t have this long lag time. And this is, I think, what’s creating excitement.”
Maybe too much.
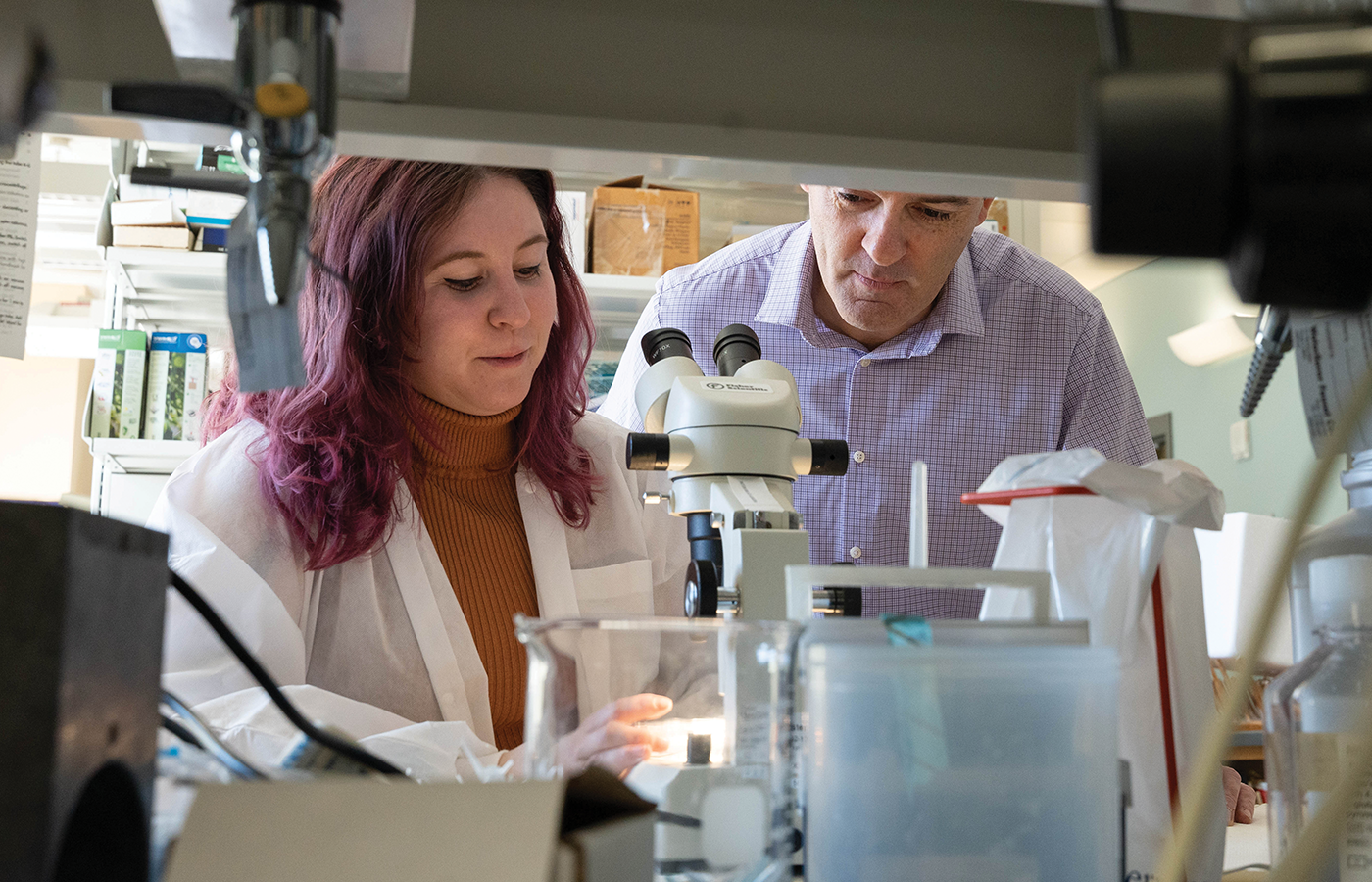
Javier González-Maeso works with Alaina Jaster, a Ph.D. student in his 10-person lab, which the National Institutes of Health has funded since 2009. (Jud Froelich)
Psychedelic therapy has become unconditionally sexy. In 2022, Netflix debuted a miniseries on the subject based on Michael Pollan’s 2018 book “How to Change Your Mind.” In February, John Oliver covered it in a 21-minute segment on HBO’s “Last Week Tonight.” Microdosing (taking a fraction of a standard dose therapeutically a few times a week) is popular and articles are just about everywhere about the healing powers of psychedelics.
But, alas, there’s frequently a lack of context and restraint in all this attention. These drugs are not a panacea from the heavens, and Alaina Jaster says more news coverage should say that.
Jaster is a 26-year-old Ph.D. student in González-Maeso’s lab and co-hosts, with fellow doctoral student Zarmeen Zahid of the University of Wisconsin, the podcast “Your Brain on Science.”
“There’s definitely an overhype with the way that things are phrased,” Jaster says. “Because you want people to click your article. I get it. But the general population probably does not read the whole article. They read the headline and maybe like a couple of paragraphs,
which sucks.
“A lot of people don’t mention — hey, this is a really controlled study where these people have been seeing a therapist for three to four weeks before their psychedelic session. They have safety nets, so if somebody freaks out, they can take care of it,” says Jaster, who in December will defend her dissertation, which focuses on using psychedelics to prevent opioid-abuse relapses by reducing cravings. She’s also studying whether sex/gender affects psychedelic experience.
Bad trips happen. Psychonauts speak of the “set and setting” of a psychedelic experience. “Set” is where your mind is when you trip, and “setting” is the environment. Both should be in order before you blast off, because psychedelics can amplify whatever’s going on around you and inside your mind. If you’re somewhere you’re not comfortable or you’re feeling distressed or unsettled, you’re risking a bad trip.
“They don’t mention these things in articles, typically,” Jaster says. “They just say psilocybin rewires your depressed brain. So a depressed person sees that and says, ‘Oh, where can I get psilocybin?’ and doesn’t know the dose they’re taking, doesn’t know all the important things that go into the trip. It’s not just, ‘Hey, this will fix you.’”
There is a lot of miracle cure propaganda today, as there was a lot of dire and scary propaganda — drug-induced insanity, notably — by the end of the 1960s, after the drugs seeped more widely into general circulation.
These chemicals, whose use in some cases has a prehistoric and sacred provenance, fueled the 1960s counterculture movement, which fueled a smear campaign leading to 1971’s Controlled Substances Act. This hunk of legislation, created in the image of Harry Anslinger and signed by President Nixon, passed a few months after the United Nations’ Convention on Psychedelic Substances, a summit in Vienna about thwarting the worldwide recreational and medical use of the nouveau cool psychotropic drugs.
The Controlled Substance Act delineated substances by danger levels — the now-ubiquitous “schedules.” Psychedelics drew Schedule I, which is for drugs considered to have no medicinal value. Psychedelics joined heroin (and marijuana) in that despised tier. Opioids — now killing thousands nationwide and the reason one pharmaceutical company is paying $6 billion in settlement money — drew Schedule II, alongside cocaine.
This was not good for psychedelic science (or, presumably, the tie-dyed T-shirt industry). Psychedelic therapy research slipped out of vogue and languished until the early 2000s. It got really hot and happening in the past five or six years, thanks in part to the more nuanced public opinions that have led to marijuana legalization in 21 states. There’s also better public relations. One evangelizing nonprofit, the Multidisciplinary Association for Psychedelic Studies, has been especially active.
“I asked [a Johns Hopkins professor] how I could become a psychedelic researcher,” says Jaster, recalling how she came to work in González-Maeso’s lab after finishing her bachelor’s at Central Michigan University. “And he told me that I should focus on learning the techniques and learning the stuff surrounding psychedelics, not just jumping into trying to find a lab that does psychedelic research, because that was 2018, 2019, so it wasn’t that popular yet. When I was looking for a lab, I would just look up things like ‘serotonin,’ ‘dopamine,’ ‘frontal cortex’ — trying to look up those keywords so I could get exposed to research in a way that was near to psychedelics but not exactly.
“There was a lot of stigma surrounding psychedelics,” Jaster continues. “A lot of the [principal investigators] at the time weren’t really advertising that they were doing that research because funding is limited for it, and it just wasn’t popular. Now, that’s totally different. You can talk about it. When I was in undergrad, I’d tell people what I wanted to do, and they’d give me a dirty look and be like, ‘You’re just like a drug addict.’ Literally, no. But OK, thank you.”
The medicinal and ritual use of plant-derived psychedelics like psilocybin and mescaline, which occurs in species of cactuses, goes back more than 5,000 years to the smudgy line dividing us from prehistory. (The Spanish conquistadors, those noted mycologists, observed the ceremonial use of magic mushrooms in 16th-century Mesoamerica.) Now, in what sometimes seem to be more enlightened times, support is growing to explore the medicinal properties of psychedelics, which have a special place in the pharmacological pantheon. No other drugs have such a transcendental pedigree. They have been reported to bring on encounters with living colors, cosmic euphoria and an all-but-ineffable sense of pantheistic love. These experiences can endure when the chemicals ebb away, leaving us to wonder: Is it the trip that helps us, all that mysterious biochemistry, or both?
“I definitely think the spiritual aspect of it is real,” says Jaster, who got into psychedelic research because of a lifelong interest in neuroscience and her experience with a family member’s alcoholism. “I would say for some people that’s necessary for the outcome — whatever they’re looking for, whether it’s by themselves in a spiritual setting or in a therapy setting. The experience as a whole is, for lack of a better word, powerful. It’s something that a lot of people can’t describe, right? And so I think that overall experience is important for some people, and I think that speaks volumes to individualized medicine in general — with or without psychedelics. Everyone’s experience is different, and what they get out of that experience is different and that's why we have some people who don’t respond to psychedelics and why we have some people who say it’s the best thing that ever happened to them.”
That’s as close as Jaster will veer toward miracles. González-Maeso’s lab moves on figures, facts and stats.
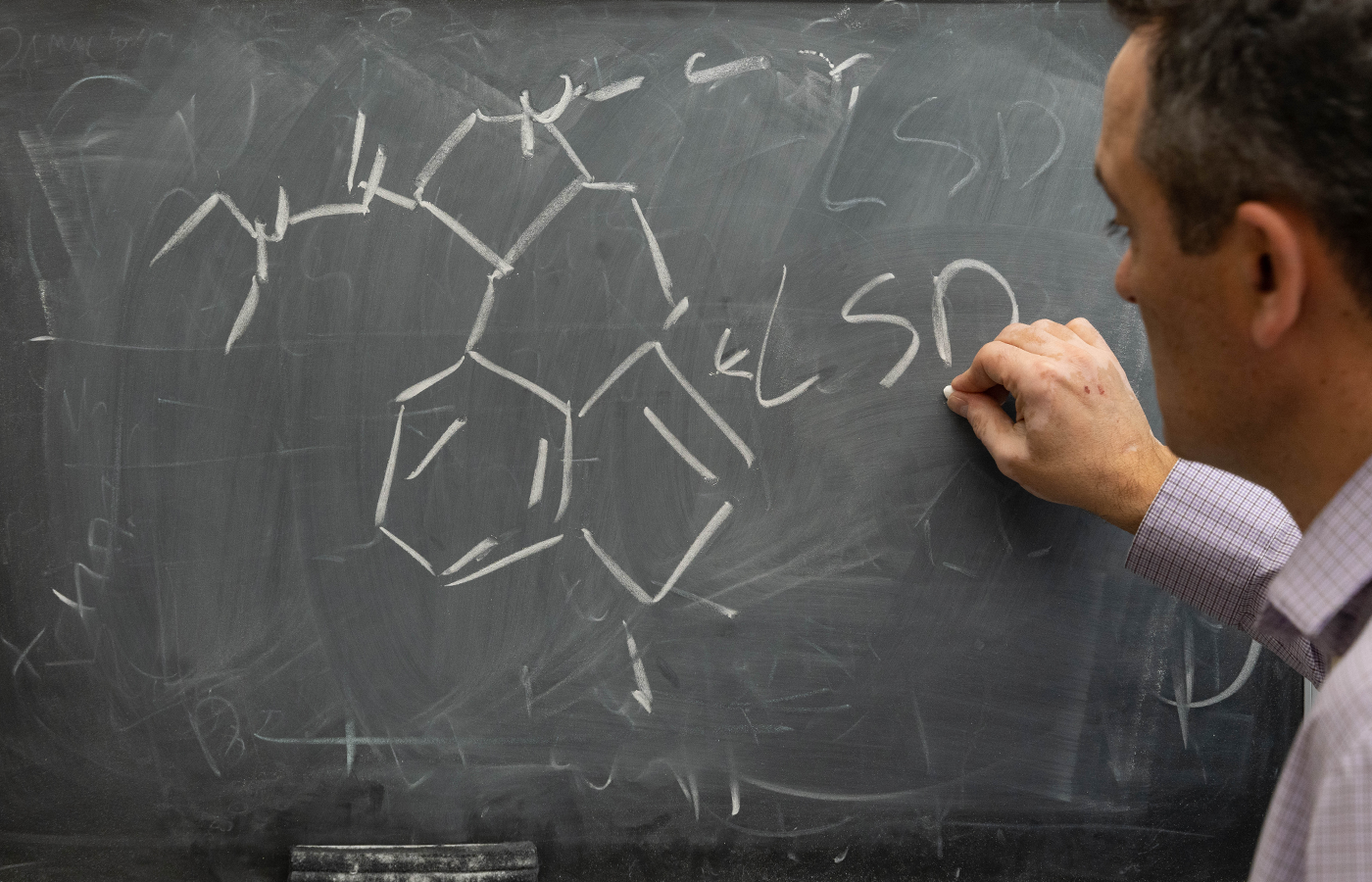
Javier González-Maeso diagrams the chemical structure of LSD, a compound commonly known as “acid” and one of the four “classical” psychedelics. (Jud Froelich)
Cool data.
It’s become a little catchphrase for González-Maeso, often accompanied by a smiley face and typed in emails to his postdoctoral students (he has two) and Ph.D. students (he has four) when their research goes somewhere no research has gone before.
“Our lab is very data-driven. He is very data-driven,” says Jaster, whom González-Maeso encouraged to check out the sex/gender differences in psychedelic experiences. “Whenever he hears somebody ask one of those ‘Do you think psilocybin could cure this?’ questions, he’s like, ‘The data’s not there yet. We’ve got to wait for the data.’ I do definitely admire that about him. He’s not going to be someone that overhypes the results or inflates the findings. He’s very matter-of-fact but he’s also really excited about what he does.”
The González-Maeso lab recently published a paper in the journal Cell Reports showing that psychedelics rewire the brain, which might lead to a new approach to alleviate depression and anxiety disorders.
Using mice, who demonstrate a drug’s effects by twitching their heads, the study found that structurally different psychedelics activate the serotonin 5-HT2A receptor differently, meaning the way these compounds bind to that receptor determines what happens (the trip) in your brain.
The interactions between drugs and receptors is a big slice of González-Maeso’s research. So far, one of his biggest breakthroughs is related to identifying an interaction at a molecular level between two receptors that recognize serotonin and glutamate (another neurotransmitter). Glutamates are involved in fundamental processes related to perception and cognition and are affected in the brains of people with schizophrenia.
González-Maeso started studying all this during his Ph.D. years and later his postdoc at the Icahn School of Medicine at Mount Sinai health system in New York City. He studied brain samples of people with depression or addiction or who died by suicide, and he noticed
that their brains were molecularly different.
This led to an interest in the chemistry of drug addiction and mental illness, and how drugs that are almost chemically identical affect brain receptors in different ways. One such drug is lisuride, which is used to treat Parkinson’s disease and is structurally similar to LSD but doesn’t make you hallucinate.
At Mount Sinai in the early 2000s, González-Maeso confirmed what Glennon proposed in 1984 about the serotonin 5-HT2A receptor: It does facilitate psychedelia in our brains and is the main molecular target for these drugs.
González-Maeso genetically modified mice to not have a 2A receptor — this wasn’t possible in the ’80s — and found that the mice behaved normally in every way except they didn’t respond to psychedelics, including LSD, psilocybin and mescaline.
“The project he worked on as a postdoc was a really hard project,” says Stuart Sealfon, M.D., a professor of neurology, neuroscience and pharmacological sciences at Mount Sinai, where he served as González-Maeso’s postdoc adviser from 2001-05. “People have been working on this problem for 50 years, and … almost a tremendous amount of what was thought about this was not consistent at all with what we found. And I think our evidence was very strong in terms of what the target was — how these drugs actually work, where in the brain they were acting. … Javier took this through from initially identifying patterns of responses to ultimately identifying the brain target for these chemicals.”
“Our lab is very data-driven. He is very data-driven. Whenever he hears somebody ask one of those ‘Do you think psilocybin could cure this?’ questions, he’s like, ‘The data’s not there yet. We’ve got to wait for the data.’”
González-Maeso earned his Ph.D. at the University of Basque Country in Bilbao in northern Spain, about 75 miles from the French border. After spending a year at Cambridge as a visiting Ph.D. student, he went to Mount Sinai, where he eventually became an assistant professor and met his wife, Paula Bos, Ph.D., who is an assistant professor in VCU’s Department of Pathology and a cancer researcher. González-Maeso arrived at VCU in 2015.
“He works quickly, he works hard, but he doesn’t rush,” Sealfon says of González-Maeso. “He’s really thorough, and he will do everything that needs to be done, and that’s a great skill. A lot of people don’t have that temperament who are in science.
“You can’t imagine how much work this is. You just can’t imagine. It’s long days of work for years and years and years, and until you get to the end, you don’t even know what you have or whether it will hold up. Through the process, you don’t know that you will get anything out of what you’re doing because until you’ve completed the study, you don’t have proof. … And, in fact, you may blow holes in your thinking at any point along the way. Science is very hard work. The hours and the intellectual effort required and the perseverance required to do it right and do it well and do important work. It’s hard. And Javier has a great temperament.”
Back at the chalkboard in his office — down the hall from his lab, it has a big window, a microscope from the 1800s and a framed painting from his then-4-year-old daughter Mailen’s nonrepresentational period — González-Maeso is finishing his SSRI diagram. It’s thorough and artistic and it greases a segue back to his ultimate mission in biological psychiatry: making better antidepressants.
“They were not looking for antidepressants. They were not looking for antipsychotics,” González-Maeso says of psychiatric drugs’ serendipitous development. “For example, in schizophrenia, the very first antipsychotic — named chlorpromazine — they were looking for an anti-inflammatory. That was in the ’50s. In that trial, they realized that people with schizophrenia who received that drug saw less psychosis, so that’s why they used that drug as an antipsychotic — and almost all the drugs that we have now, since then, are based on that one. … We need to identify new chemical compounds and find new ways to treat the disorder.
“Since my Ph.D. days, I’ve been combining pharmacology — how drugs affect behavior — [and] psychiatric conditions: depression, opioid abuse and schizophrenia and those things,” he continues. “Something that I still think is an important question and what I also tell to the students when, many times, they ask me: Why are you interested in psychiatry if you are not a clinician, if you are not a psychiatrist? Well, I can tell you many of us have psychiatric conditions. … We are supposed to bring some of the knowledge that we generate back to society, and eventually we can find new treatments, cure diseases.
“If you model depression, if you model drug abuse, if you model alcoholism, the parts of the brain affected by these drugs, they affect differently different parts of the brain. So again, what part of the brain is responsible for these behaviors? I mean, that is the only question.”
And how much of this remains brain magic to biochemists, affably Spanish and otherwise?
“Almost all of it.”
