Research & Discovery
A sound treatment
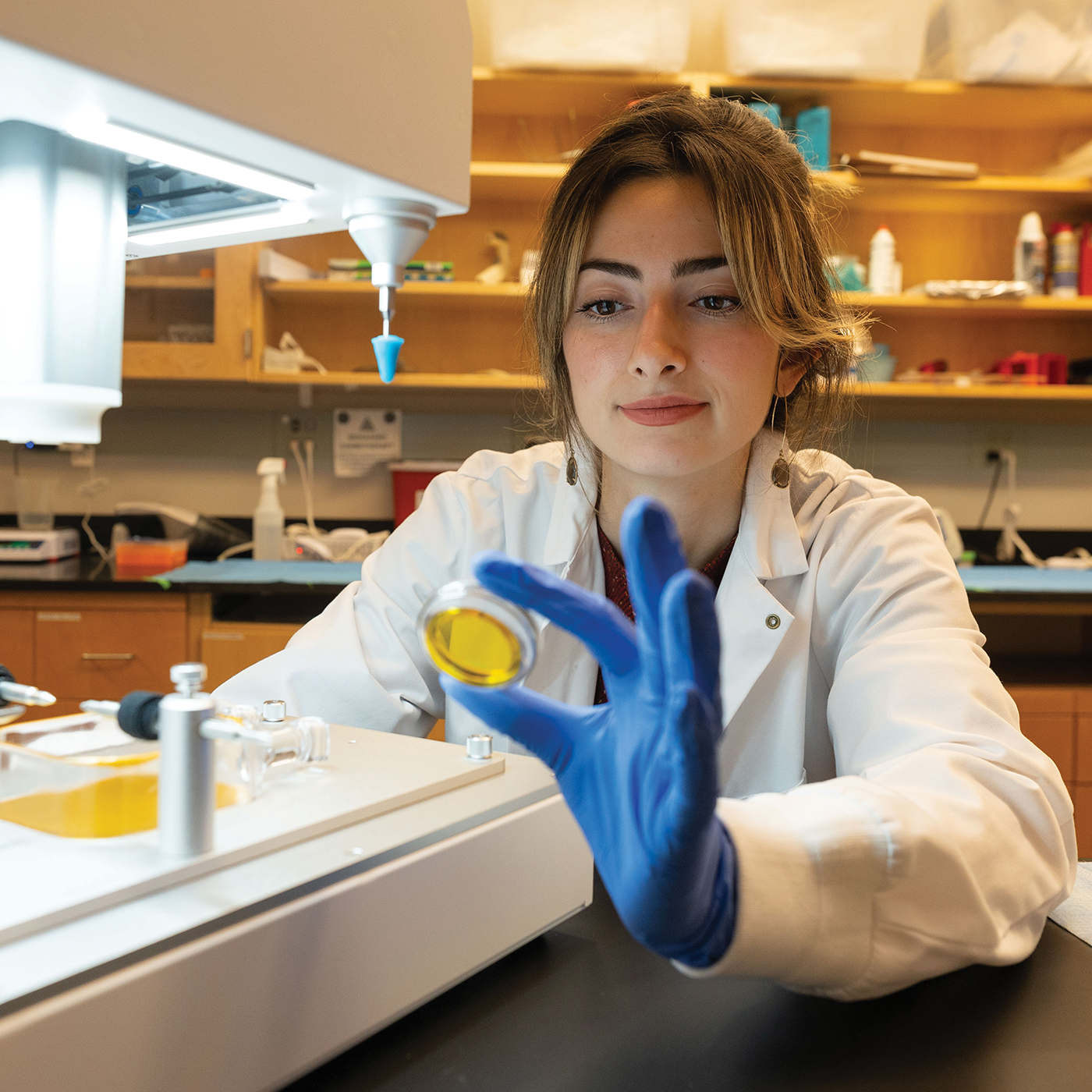
Known as a diagnostic tool, ultrasound has a therapeutic side. Natasha Sheybani (B.S.’15) is using it to fight tumors.
When Natasha Sheybani, Ph.D. (B.S.’15), talks about focused ultrasound therapy, her voice rises excitedly and her sentences dance together in a melange of technical terms and everyday metaphors. The assistant professor of biomedical engineering at the University of Virginia appreciates how nuanced the field has become.
Ultrasound is universally known as a medical diagnostic tool. It works by transmitting high-frequency sound waves into the body, which “bounce back” as echoes and then are converted to images. But the past few decades, Sheybani says, have yielded immense therapeutic potential for a technology we normally associate with pregnancy and peering into organs such as the liver and pancreas.
“Focused ultrasound is an emerging strategy for concentrating sound waves and pinpointing them to a single location within the body,” she says. “It is at that location, where all the acoustic energy coalesces, where we can yield a versatile array of impacts to targeted issues.”
Sound is energy, Sheybani continues, and when a focused ultrasound researcher tunes sound waves and points them toward a single small area like a patch of tissue, one thing all that energy can do is generate a lot of heat. It’s akin to using a magnifying glass to focus sunlight and burn a hole in a leaf — but instead of a leaf, focused ultra- sound can dial up sound-generated heat on tissue ravaged by cancer, effectively eliminating or damaging it.
At its highest intensities, focused ultrasound can burn cancerous tissues or trigger the formation of bubble clouds from gases naturally present in tissues, which then oscillate and eventually col- lapse, destroying the tumor in a process called ablation.
Sheybani’s lab is studying how this laserlike harnessing of ultrasound waves across varying intensities can improve how we treat metastatic breast cancer and brain tumors. For decades, we’ve battled these aggressive cancers with surgery, radiation and chemotherapy drugs that save lives but have side effects like heart dam- age, neuropathy and brain fog. Alongside immunotherapy and antibody-drug conjugates that seek and destroy specific cancer cells, focused ultrasound offers a spatially precise, noninvasive approach.
The therapy is relatively niche. (Sheybani is also the research director of UVA’s Focused Ultrasound Cancer Immunotherapy Center, which opened in 2022 and bills itself as the first of its kind in the world.) But it’s not new. In 1955, brothers William and Francis Fry used the technique to perform a partial ablation to remove a brain tumor. In the 1960s, William Fry used it to treat patients with Parkinson’s disease.
Today, research trials are studying focused ultrasound’s potential to treat Alzheimer’s disease, drug addiction, essential tremor (a movement disorder) and brain cancer. That versatility is exciting scientists like Sheybani and the institutions that reward their breakthroughs.
In 2018, three years after graduating from VCU’s College of Engineering, Sheybani, then pursuing her Ph.D. at UVA, became the first at her institution to earn a grant from the National Cancer Institute to support her transition from predoctoral to postdoctoral studies in cancer research. In 2021, while a postdoc at Stanford, she received the Director’s Early Independence Award from the National Institutes of Health, a five-year, $1.25 million grant that fast-tracked the launch of her lab. Last year, she landed a spot on Forbes’ annual 30 Under 30 list in the science category.
Sheybani’s 10-person lab today is flush with assistants and equipment. She’s running a half-dozen preclinical projects and supporting three clinical trials. And UVA’s focused ultrasound center is running a trial that pairs ultrasound ablation and low-dose chemotherapy in patients with early-stage breast cancer, spun out of research Sheybani did as a Ph.D. student.
Some of Sheybani’s studies deploy focused ultrasound as a delivery vehicle or “beacon” for cancer treatments. Sheybani refers to these as a few of the technology’s “mechanical” benefits (versus the “thermal” benefits it offers as a tumor-destroying sound beam).
For example, her lab is studying how focused ultrasound can target or augment drug delivery by opening temporary gaps in the blood-brain barrier, the shrink-wrap- like network of vessels throughout the brain that ordinarily protects it from harmful substances like circulating toxins or pathogens. “It’s designed to keep bad things out,” Sheybani says, “and the challenge is that it renders the brain pharmacologically privileged,” essentially blocking medicine from getting into the brain.
For people with brain tumors, that means drugs don’t reach their target. But with low-intensity focused ultrasound, Sheybani can bore holes in the barrier “to safely and noninvasively enable the pas- sage of important therapeutics into the brain, following which the barrier recovers,” she says — usually within 24 hours.
Sheybani is also exploring focused ultrasound’s reconnaissance potential. Some tumors, though visible on a scan, evade the body’s immune response, and focused ultrasound has the potential to unmask these veiled cancer cells, guiding immune cells and cancer-fighting drugs to the right place and unleashing them.
“Cancer is remarkably skilled at masking itself from the immune system, which is always scanning our bodies for signs of danger,” she says. “We envision using therapeutic sound waves to lift off the mask, mobilizing the immune system to recognize that cancer is in the body and to effectively mount a response against it.”
